FAQs: Imaging
Breast Imaging
What is a mammogram?
A mammogram is a radiographic image that gives a picture of the internal structure of the breast. There are two types of mammography: screening and diagnostic.
A screening mammogram is performed on women who have no evidence of breast disease. Using a mammography machine, a radiologic technologist obtains two views of each breast. Screening mammography is the best way to detect breast cancer early. A screening mammogram is similar to other screening exams such as a PAP smear, PSA for prostate cancer, fecal occult blood to detect colon cancer and a glucose test to detect diabetes.
Yearly screening mammography should be a routine procedure for all women ages 40 and older. Women with a strong family history (mother, sister or daughter) of premenopausal breast cancer may wish to begin screening earlier.
Diagnostic mammography is performed when a possible abnormality, such as a lump, has been found on a screening mammogram or upon clinical examination of the breast. It includes special views in order to better evaluate the abnormality. A diagnostic mammogram is read by the radiologist at the time of the exam.
Who is the radiologist?
Radiologists are physicians who specialize in all aspects of imaging the body. This includes exams used to diagnose abnormalities and in performing biopsies of tissues that require imaging guidance (example: biopsies of breast lesions that cannot be felt). Radiologists understand radiation safety issues and the methods by which images are acquired, which makes them uniquely qualified to interpret imaging studies and to perform image guided biopsies.
Radiologists have 4-6 years of specialized training after earning a medical degree. Those who read mammograms have additional training solely devoted to breast imaging. To maintain certification to read mammograms, the radiologist must read many mammograms a year, maintain continuing education credits pertinent to mammography and are subjected to medical audits. Statistical results are compared to local and national results.
What does it mean to have an "abnormal" mammogram?
A finding on your screening mammogram requires further evaluation to determine if it is suspicious. This evaluation usually involves specialized mammographic views. It may require physical exam, ultrasound or an MRI exam. Most of these “abnormal” findings can be resolved as benign (not cancer) on subsequent imaging. If they cannot be resolved as benign, then a follow-up study or biopsy may be recommended.
Why might my doctor recommend a 6 month follow-up exam for an abnormal finding?
A six-month follow-up may help to avoid unnecessary biopsies.
Almost all women have lumps, calcifications or abnormal densities on their mammograms. The radiologist assesses the risk that these may be cancer based on their appearance, the patient’s age, clinical history, use of estrogen, family history, and whether or not the abnormality has changed compared with prior mammograms. This is why it is so important to have your previous mammograms available.
After thorough assessment, if the radiologist finds no suspicious features, he/she may recommend a follow-up study in 6 and 12 months to make sure the area doesn’t change. This is a well-researched, widely practiced, and acceptable method to deal with “probably benign” abnormalities.
What is the chance that an abnormality followed at 6 and 12 months is really a cancer?
This does happen, but it is uncommon. These “probably benign” findings have been well-researched. For example, in a research study involving thousands of women being followed for probably benign masses, only 1.7% were ultimately found to be cancer. These were diagnosed because they grew on the follow-up studies and were eventually biopsied. One-third of these had grown at the six month study, 1/3 did not show growth until the 12 month study, and 1/3 did not show growth until the 24 month study. Because “benign” appearing cancers are usually the slow-growing variety, these patients still presented with early stage cancers (same prognosis as if biopsied initially).
The six-month follow-up practice is used to prevent many unnecessary biopsies.
XRay/Fluoroscopy
What is Diagnostic Radiology/Fluoroscopy?

Diagnostic radiology is the examination of the tissues and deep structures of the body by X-ray. Fluoroscopy allows the physician to obtain “live” X-ray images and view them on a television screen.
What are some Diagnostic Radiology/Fluoroscopy services?
- Upper GI Series
- Air Contrast Colon
- Intravenous Pyelogram (IVP)
- Small Bowl Enteroclysis
- Fluoroscopic Guided Biopsy
- Arthography
- Myelography
- Modified Barium Swallow
- Hystersalpingogram
- Venogram
Nuclear Medicine
What is Nuclear Medicine?

Nuclear medicine is a subspecialty within radiology. It comprises diagnostic examinations that result in images of body anatomy and function. The images are developed based on the detection of energy emitted from a radioactive substance given to the patient, either intravenously or by mouth. Generally, radiation to the patient is similar to that resulting from standard X-ray examinations.
What are the use for Nuclear Medicine?
The list below includes many of the nuclear medicine examinations available.
- Myocardial Perfusion Scan (a.k.a. Exercise/Pharmacologic Stress Scan)
- Bone Scan
- Hepatobiliary Scan
- Lung Scan
- Renal Scan for High Blood Pressure or Captopril Renogram
- Thyroid Scan and Iodine Uptake
- White Blood Cell Scan
- Galium Scan
- GI Bleeding Scan
- Gastric Emptying Study
- Parathyroid Scan
- Oncoscint
- Octreoscan
- Nuclearcisternogram
PET/CT Scan
What is a PET scan?
PET is a nuclear medicine technique, which captures images of the human body’s function and reveals information about disease. With PET scan imaging, physicians can collect images of function throughout the entire body, uncovering abnormalities that might otherwise go undetected. No other imaging technique shows the internal metabolism of the body so well. Often times, PET can detect and stage most cancers before they are evident through other tests such as X-ray, MRI, and CT scan. PETalso can give physicians important information about heart viability and neurological disorders, such as Alzheimer’s, seizure disorders and brain tumors.
PET is a reliable, non-invasive way to tell whether or not a tumor is benign or malignant. PET scan imaging evaluates for cancer in a single examination, which allows physicians to stage a cancer and to suggest treatment options earlier, which may spare patients expensive and often painful surgical procedures.
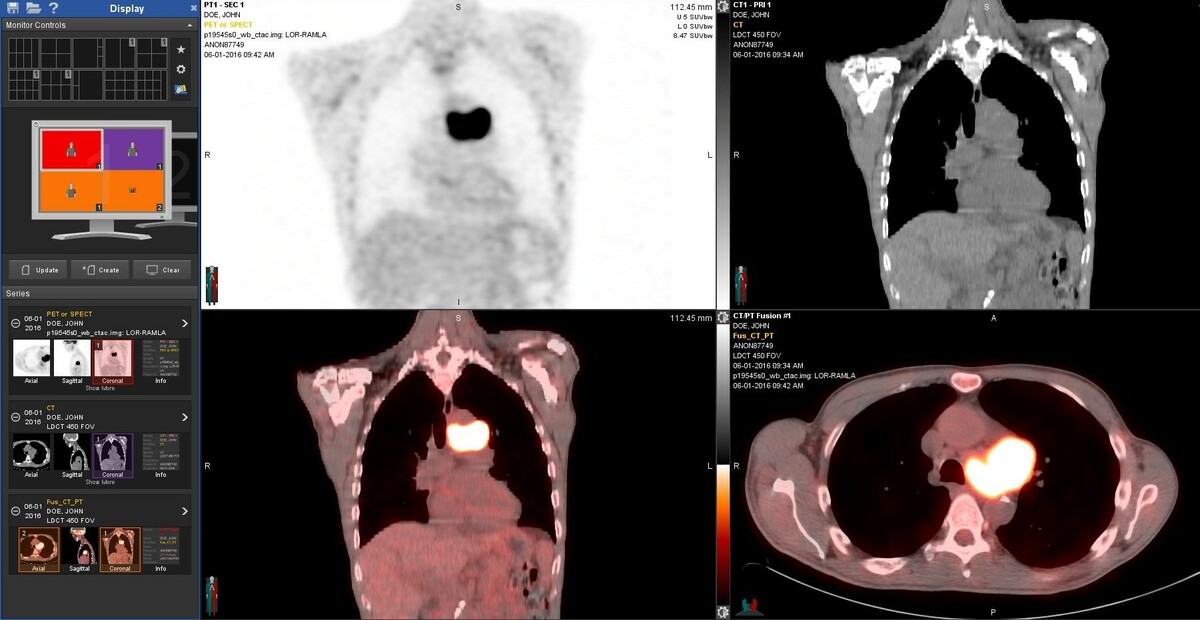
How does PET work?
When disease strikes, the metabolism of tissues and cells changes. Using a tracer drug to highlight areas within the body, a PET scan picks up a signal from the organs. If an area in an organ is abnormal, the metabolism will be different than in the surrounding tissues. This data is computer processed and made into images.
What should I expect during my PET scan?
Specific instructions will be given to you at the time you are scheduled for your PET scan. In most cases, we will ask you not to eat or drink anything for 8-12 hours prior to your scan. If you are diabetic, please inform the PETstaff so special arrangements can be made to meet your specific needs.
PET procedures routinely require an intravenous injection of the tracer material. This necessitates a needle stick in an arm or hand vein, much like when having a blood sample drawn or when getting an “IV” line.
During the PET scan, you must lie down and remain very still for varying amounts of time, depending upon the procedure chosen for you. Some patients get stiff from keeping still, while others may fall asleep. The technologist performing the study will go over the procedure intended, so you will know the details of what to expect and what is expected of you.
Will my PET Scan be covered by my insurance?
Medicare as well as many third party payers reimburse for PETscans.
The most recent Medicare policy covers PET scans of the following cancer groups:
- Diagnosis, staging and re-staging of non-small cell lung cancer
- Diagnosis, staging and re-staging of colorectal cancer
- Diagnosis, staging and re-staging of cervical cancer
- Diagnosis, staging and re-staging of esophageal cancer
- Diagnosis, staging and re-staging of melanoma (not covered for the evaluation of regional lymph nodes)
- Diagnosis, staging and re-staging of head and neck cancers (not covered for central nervous system or thyroid cancers)
- Staging and re-staging of breast cancer
- Characterization of solitary pulmonary nodules (SPNs)
- Diagnosis, staging and re-staging of lymphoma
- Restaging of recurrent/residual thyroid cancers after thyroidectomy and ablation under specific conditions (please contact us to find out if you meet the specific requirements to qualify)
PET is not covered for other diagnostic uses and is not covered for screening (testing of patients without specific symptoms).
DEXA Bone Density Scan
What is a DEXA exam?
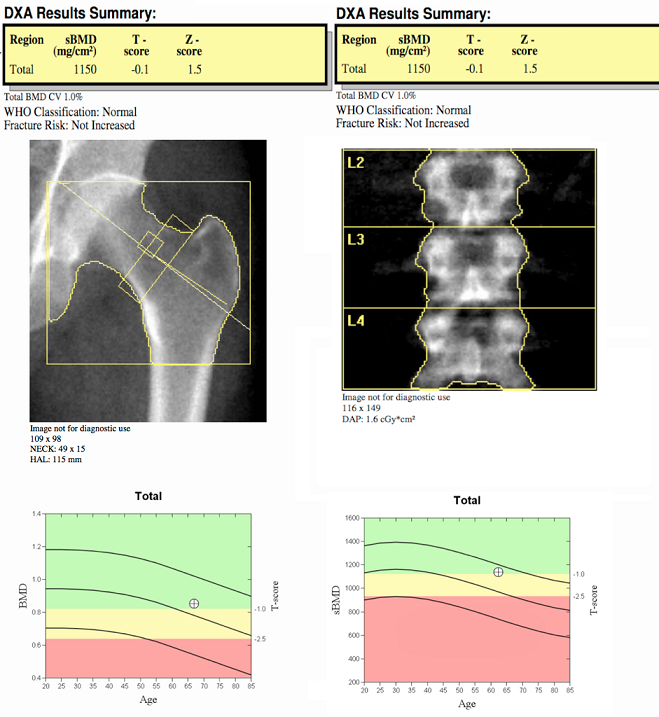
Full-body DEXA exams are offered at our hospital imaging centers. Bone densitometry, using DEXA (dual-energy X-ray absorptiometry), safely, accurately and painlessly measures bone density and the mineral content of bone. DEXA is the most widespread, non-invasive test for the detection of osteoporosis, and is the best way to identify individuals who are at increased risk for future fractures. Based on your test results, your physician can suggest treatment options from exercise and lifestyle changes, nutritional supplements or medication. The goal of diagnosis and treatment is to prevent fractures.
Am I at risk?
Your chances of developing osteoporosis are greater if you are female and answer “yes” to any of the following questions:
- Are you…?
- Light skinned
- Thin or small framed
- Approaching or past menopause
- Milk intolerant or have a low calcium intake
- A cigarette smoker or drink alcohol in excess
- Taking thyroid medication or steroid-based drugs for asthma, arthritis or cancer; this includes individuals suffering from hyper-thyroidism and hyper-parathyroidism
- Do you have…?
- A family history of osteoporosis
- Early, natural or surgical menopause (i.e. hysterectomy)
- Long term steroid use (for conditions such as asthma and arthritis)
- Chronic intestinal disorders (i.e. malabsorption syndrome, post-gastrectomy)
- Rheumatoid arthritis
- A sedentary lifestyle
How do I prepare for a DEXA exam?
Unless otherwise instructed, eat normally the day of your exam, but avoid taking calcium supplements for at least 24 hours prior to your appointment. Wear loose, comfortable clothing. Sweat suits and other casual attire without zippers, buttons or metal objects are preferred.
You should not have had a barium study, radioisotope injection, oral or intravenous contrast material from a CT scan or MRI within seven days prior to your DEXA test.
Ultrasound
What is Ultrasound?
Ultrasound (US), also called ultrasound sonography, is a method of obtaining images from inside the human body through the use of high frequency sound waves. The reflected soundwave echoes are recorded and displayed as a real-time visual image. No ionizing radiation (or x-ray) is involved in ultrasound imaging.

What are the uses for Ultrasound?
The list below includes some of the many uses of ultrasound.
- Ultrasound of Neck, Chest, Abdomen and Pelvis
- Pregnancy Ultrasound
- Breast Ultrasound
- Ultrasound Guided Needle Biopsies
- Ultrasound Guided Core Biopsy of the Breast
- Doppler Ultrasound of the Abdomen
- Ultrasound Guided Prostate Biopsy